Course length 8hrs
Interactive graphics
Self Paced
6 Month Access
Course Overview
Written by Accredited Exercise Physiologist and Sports Therapist Paul Peglar, who has over 20+ years of experience in musculoskeletal rehabilitation, START Training has developed a new professional development course ‘Process for Exercise Prescription: Common Knee Dysfunctions’. This course is 100% online and self-paced.
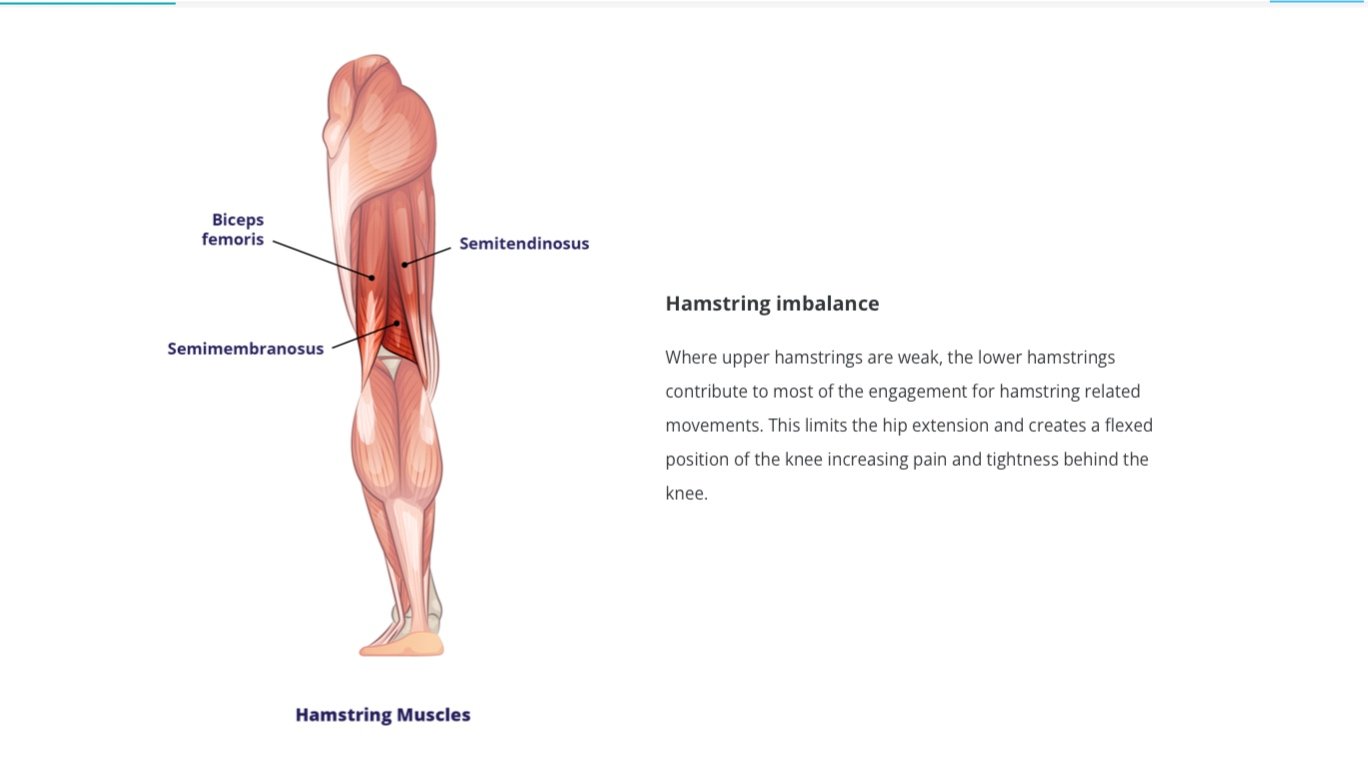
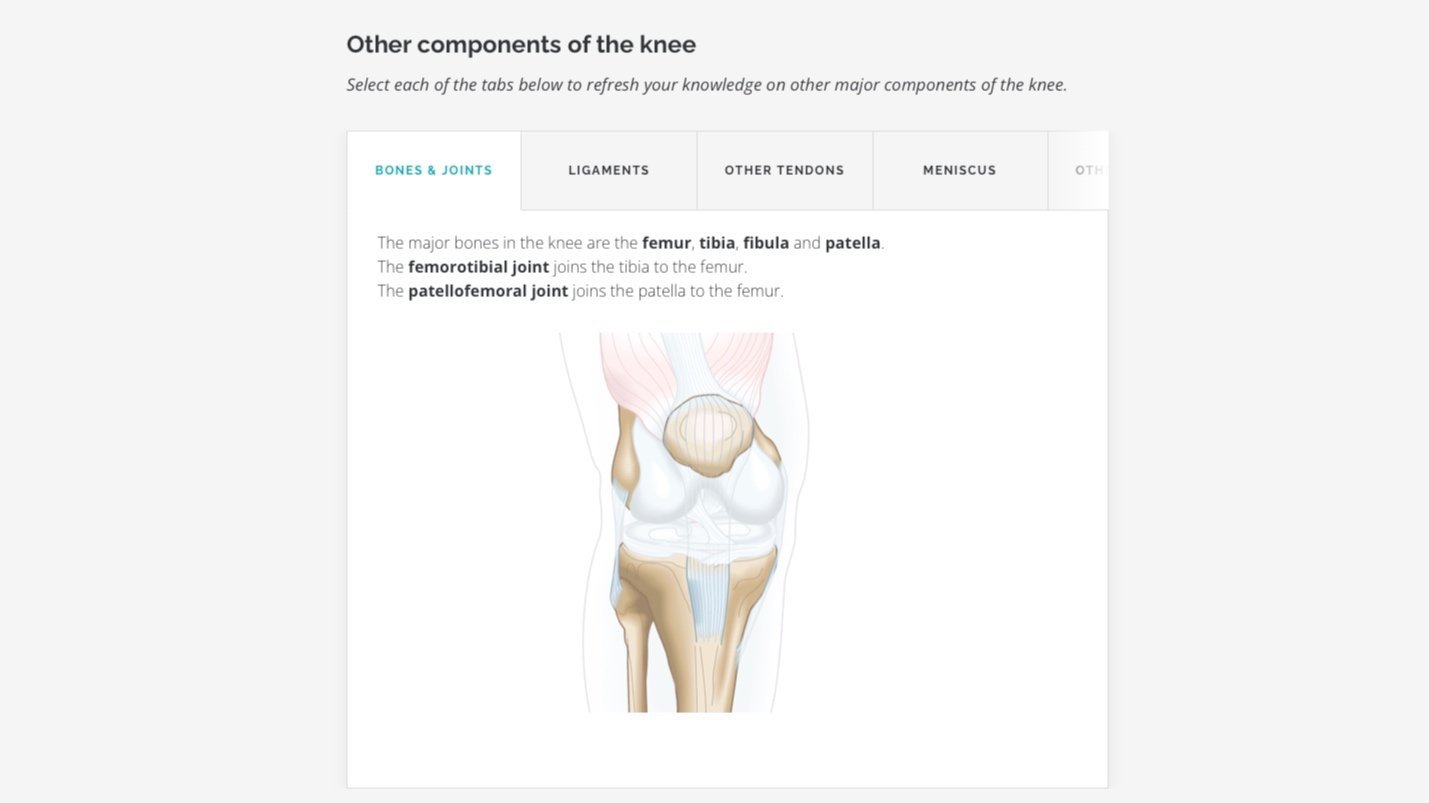
Paul reviews the functional anatomy of the knee and general exercise principles for exercise selection and programming to address common knee dysfunctions. Case studies are utilised to practically address how the role of client differential and diagnostic tests dictate exercise selection and the direction of the program.
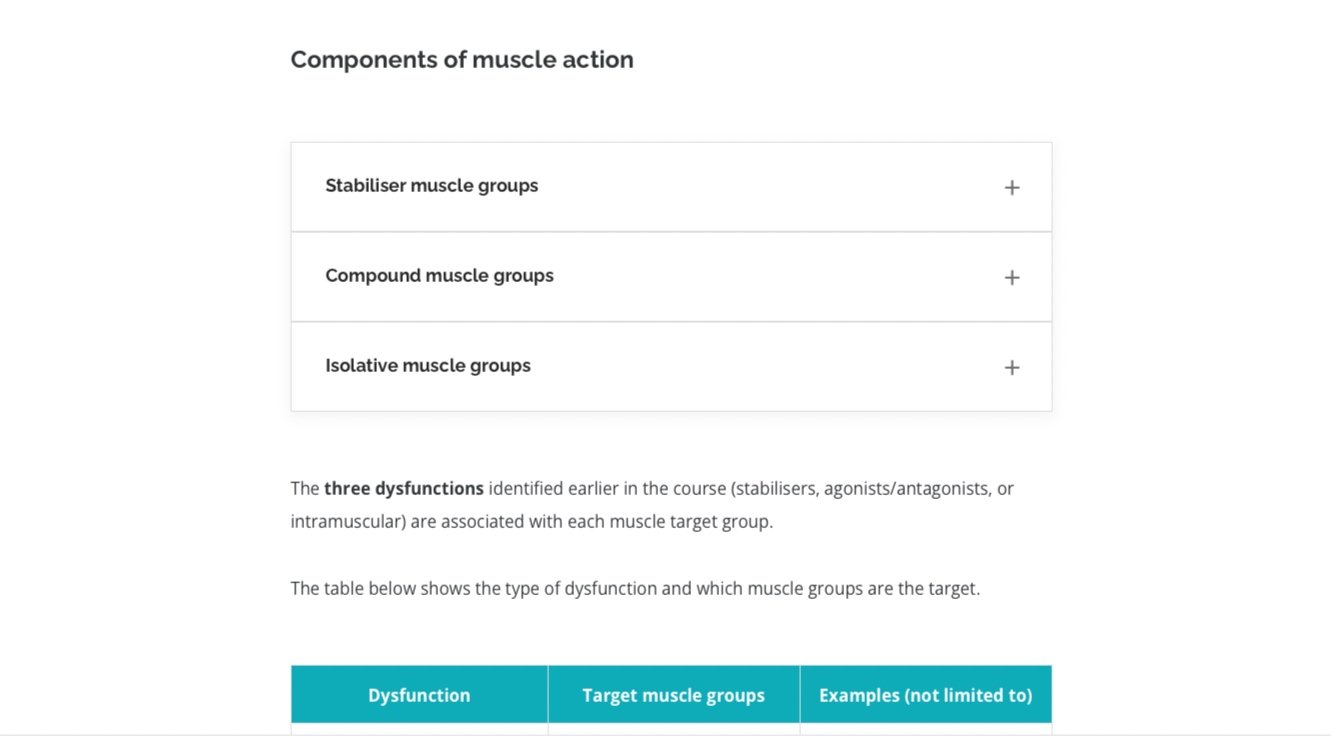
Paul presents his framework for categorising non-acute knee pain/dysfunctions which has been built upon evidence-based principles and 20+ years of experience. In this course he details how to objectively assess which dysfunction is present, whether it be an Agonist/Antagonist, Stabiliser, or Intramuscular movement dysfunction, and indicates the parameters for exercise prescription of each. The course covers why it is important to factor in the client’s training history for corrective exercise prescription where the program may prioritise muscular engagement, neural development or strengthening type exercises.
Learning Objectives
By the end of the course you will be able to:
Identify the anatomical structures of the knee joint
Understand the role of the knee in movement, stability and power
Identify common knee dysfunctions
Select the correct muscle movements to focus on when treating common knee dysfunctions
Explain exercise program considerations for specific populations and activities
Design an exercise program for a client based on their knee dysfunction and history
Justify your choice of exercise selection for each unique client.